Evaluation and management (E/M) service coding and documentation has to be the issue that physicians despise reading about the most. As we all understand, the “guidelines” for code and documentation are a tangle of regulations that encourage down coding by keeping the laws unclear and the severe penalties. The “new framework” for documentation standards, which is anticipated to be issued later this year, may or may not clarify the regulations. So far, revision hasn’t made the process any simpler to use.
According to CPT, 99214 is recommended for an “office or another outpatient visit for assessing and caring of an established patient, which needs at least two of these three essential aspects: a complete history, a thorough analysis, and medical decision making of varying capabilities.
99214 General Guidelines
Consider 99214 in any of the following circumstances:
- If the patient develops a new Problem that might result in substantial morbidity if left untreated.
- If the patient has three or more previous issues.
- If the patient develops a new issue that necessitates a medication.
- If the patient has three stable problems that need medication renewals, or if the patient has one steady-state and one poorly managed problem that requires drug refills or changes.
Documentation
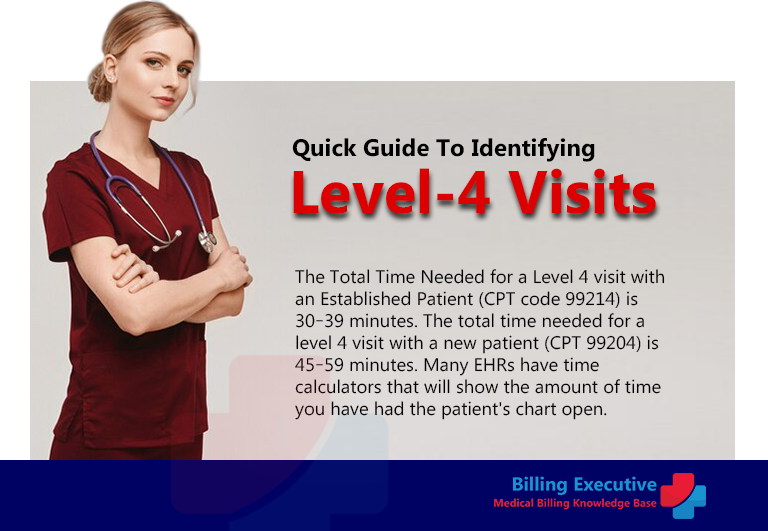
To keep our use of level-4 codes more uniform and decrease the amount of time spent on coding, I created the “Level 4 Reference Card” for myself, my colleagues, and our residents. The card’s front includes the primary requirements that your documentation must fulfil to classify a visit as a 99214 (any two of the following: a complete history, a detailed exam, and moderately tricky decision making), and it describes the materials that must be documented to satisfy each requirement. It also has a box that describes the requirements for a level-4 visit with an existing patient (99214) vary from a level-4 appointment with a new patient (99204).
The reference card can be used in at least two main ways: First, using the card attached to the wall where you dictate, you may follow along while you write your note, ensuring that your dictation contains all of the information that suggests your level-4 code option. You can also use the reference card as a guide for performing internal audits of other doctors’ records.
Internal coding and documentation audits may strike you in the same way dental appointments hit the general public, but don’t dismiss their importance. Every doctor in our 22-person group evaluates five dictations every month, and every physician is a better coder. In our practice, the physicians are expected to be the coding specialists.
It’s also crucial to enhance the quality of your coding. We’ve discovered that adding the CPT codes to the bottom of all our dictations and highlighting them on the superbills is a valuable tip. As a result, we may conduct our mini-audits to confirm that our documentation validates our coding when we receive our dictations. If we discover that we have under coded, we usually write off the penalty. If we find out that we have coded too high, we may file a corrected claim (and our procedure is to hold all our level-4 and -5 Medicare charges until the dictation has been reviewed). The actual value of this practice is that it helps all of us better coders.
Level 4 Visits With New Patients
A detailed history and physical exam are required for a 99214, whereas a complete history and physical exam are required for a 99204. In terms of documentation, the discrepancies are reflected in four ways:
- All three essential requirements (history, physical exam, and medical decision making) must be satisfied for a 99204. Only two of the three basic requirements are required for a 99214.
- The system review for a 99204 must encompass at least ten systems or bodily parts. A 99214 requires only two studies.
- The previous family and societal history for a 99204 must include all three sectors. A 99214 requires one area.
- The physical test for a 99204 must encompass at least 18 shots from at least nine systems or physical locations. At least 12 rounds from at least two systems or bodily areas are required for a 99214.
When we neglect to follow the guidelines, we may fail to include information collected during the visit in the patient record – information that we believed was important due to the patient’s condition.
About us
Billing Executive – a Medical Billing and Coding Knowledge Base for Physicians, Office staff, Medical Billers and Coders, including resources pertaining to HCPCS Codes, CPT Codes, ICD-10 billing codes, Modifiers, POS Codes, Revenue Codes, Billing Errors, Denials and Rejections.
We have more than 10 years experience in US Medical Billing and hand-on experience in Web Management, SEO, Content Marketing & Business Development with Research as a special forte.
Learn More
CPT Code Of Pain Management 2022
What is the correct way to utilize CPT CODE 99214?
Understand and Recognize the Types of CPT Codes 2022
Coders to Know Where It’s “AT” in Clean Chiropractic Claims
